Today, more than 56 000 patients in Finland (with 2500 new cases per year) are diagnosed with the chronic inflammatory bowel diseases (IBD), Ulcerative colitis or Crohn’s disease. The IBD patient numbers in Europe and North America are reaching 4 million. These cases are now rising at a worrying speed here at home especially in youth, and overall in the developing countries.
How do we as individuals and the clinicians then know if something serious is going on in the gut, or, if we are in an unusually stressful or exciting period with “butterflies in the stomach”? Nevertheless, the increasing prevalence of various gut disorders requires a major attention from both the healthcare and research communities.
To differentiate between the many gut ailments, robust, specific, easy to perform and preferably inexpensive and non-invasive biomarkers are needed. Disease modeling and defining the cellular and molecular biology behind the diseases, are necessary to understand disease development and to identify better biomarkers.
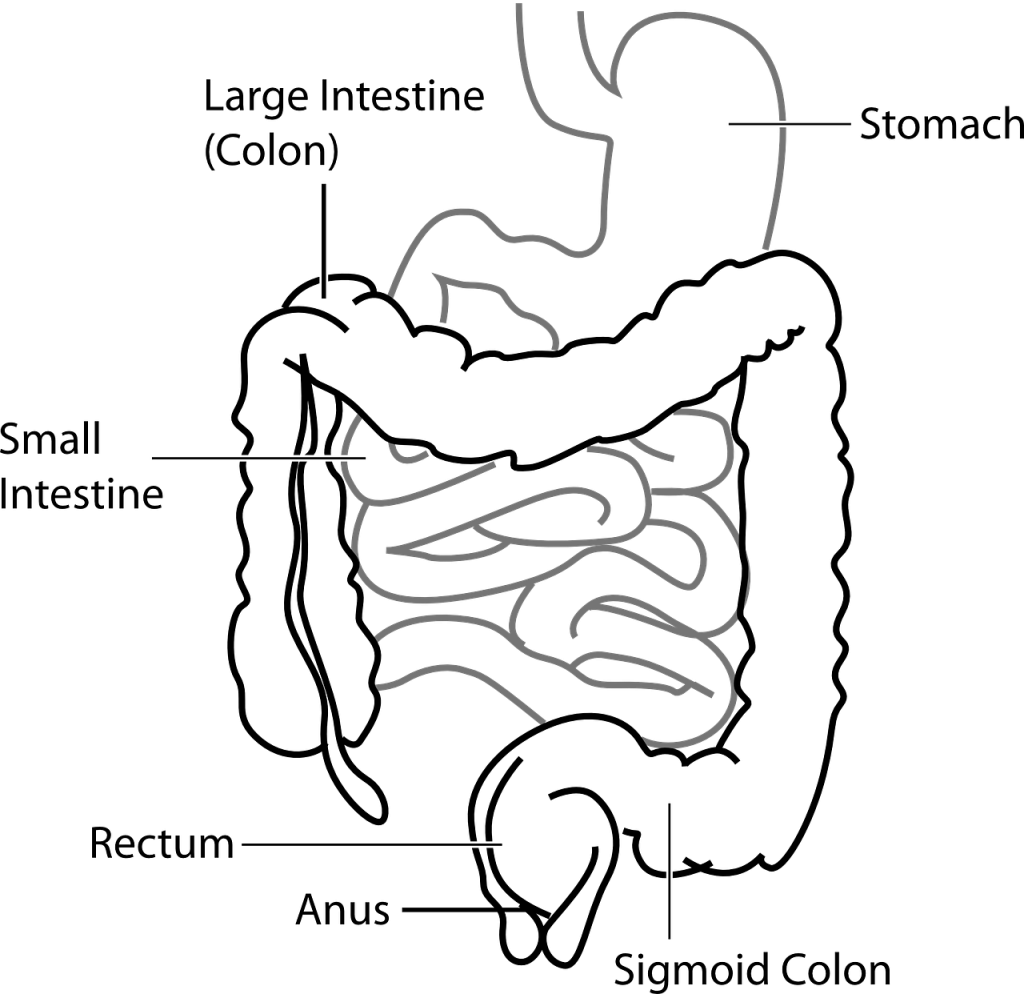
For chronic inflammatory gut disorders, diagnosis is now based on symptoms, invasive colonoscopy and pathological findings from biopsies, as well as elevated levels of stool calprotectin, which is not fully disease specific. While calprotectin measures inflammation-inducing neutrophil activity that leaks through the broken barrier, there are currently no accurate marker to measure the condition and damage of my superheroes, the intestinal epithelial cells (see InFLAMES “The Gut feeling” blog, Part 1).
Fascinating keratin family
Since my early career, I have been fascinated by the keratin family of proteins, since they are not only the static, abundant cytoskeletal cables and sample contaminants from skin and hair, that their reputation holds.
Instead, keratins form very dynamic cellular networks that can be altered in stress conditions, and that participate in regulating signaling events. The large family of over 50 keratins are expressed in a cell and tissue dependent fashion, which has led to that their prognostic value for epithelial cancers is standardized in the pathology labs since long back. Keratins are also very abundant, and thus easy to detect, adding to their many good features as biomarkers. Could then keratins be further explored for inflammatory gut ailment diagnosis?
In my team at Åbo Akademi University, we study keratins in gastrointestinal tissues mostly using pre-clinical disease models. Recently, together with our colleagues from University of Turku, the Turku university hospital, Turku PET center and Auria Biobank we have focused on several IBD -related projects using PET-imaging, histological analysis and biomarker analysis.
Using modern quantitative digital image analysis techniques, spear headed by project researcher Lauri Polari, my team has identified a less known keratin, keratin 7, that is not expressed in the healthy human colon, but that increases specifically in IBD patients but not in patients with microscopic colitis.
Towards innovations!
While we investigate the mechanisms behind this neo-expression or keratin 7, we are also evaluating the potential of this possible biomarker for non-invasive diagnostic purposes. I want to thank our universities that are building great innovation expertise to help us basic research scientists (used to look into the microscope), navigate in this field, and to our InFLAMES Flagship that both sparks and fuels the importance of innovation in immunobiology.
As a cell biologist researcher and teacher, it feels motivating for me to not only wish that our research may one day add a new sentence in a text book, but with a hopeful “gut feeling”, work towards innovations that might one day help large patient groups diagnose and monitor disease progression for better health and life quality.

Diana Toivola, Associate professor at Åbo Akademi University
Faculty of Science and Engineering, Biosciences, Cell Biology

One thought on “Gut feeling, Part 2: Butterflies in the stomach or something serious?”