Inflammatory bowel disease, ulcerative colitis, Crohn’s disease, microscopic colitis, lymphocytic colitis, collagenous colitis, leaky gut, irritable bowel syndrome, celiac disease – a long list of some of the different ailments and diseases that can occur in the intestine. Complications in diagnosing and treating these conditions, that often have a chronic inflammatory component, is due to that:
a) the underlying cellular and molecular mechanisms are poorly known,
b) several unknown sub-diseases or disease variants likely exist,
c) the causes can be multifactorial, and,
d) the diagnostic methods are often invasive and not always diseases-specific.
So, there is a lot for us scientists to do, even if we know that the old saying “An apple a day keeps the doctor away” holds a lot of truth.
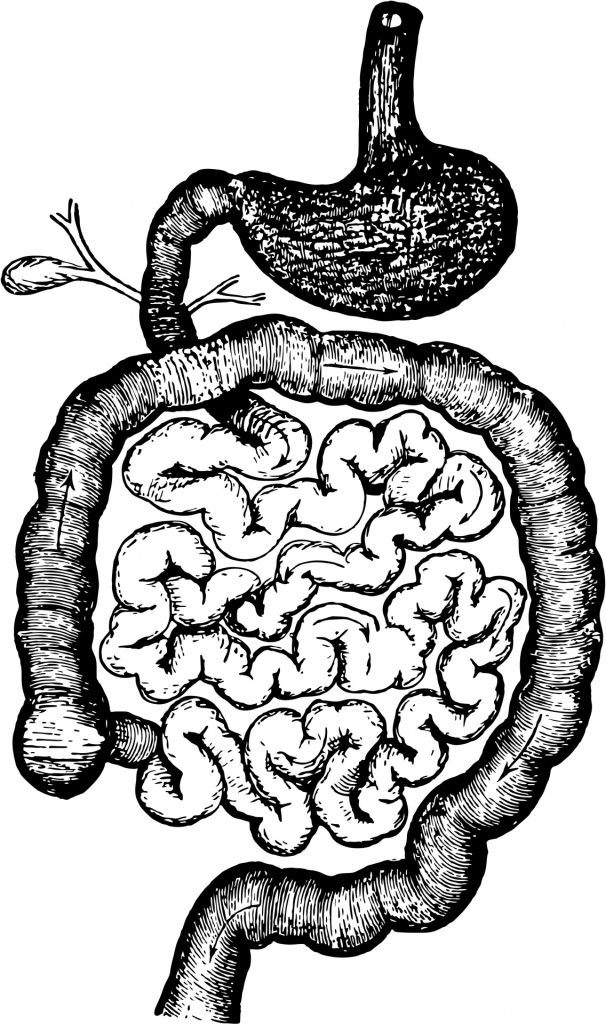
Even if the intestine runs and winds pretty much in the center of our bodies and we usually take its daily functions for granted, it is still a danger zone for our health since the central canal of the intestinal tube is in contact with the outside world in both ends.
Fortunately, there are many defense systems (mucus, immune system, defense molecules) that protect the sterile inside body beyond the gut wall, where also the nutrients from our food need to find their way to help build the components of all of our cells and organs.
My personal superheroes in the gut are the epithelial cells that line the intestinal wall facing the central canal. This amazing single-cell layer of cells connected to each other, together with the mucus they produce, build a protective barrier between the “outside” and the “inside” worlds.
Folding builds huge surface
The multiple levels of folding of the epithelium, build the intestinal mucosa and extend hugely the surface area for eg. nutrient and water uptake.
As if this that was not enough, these epithelial cell heroes of mine are very dynamic, as the stem cells at the bottom of the folds called crypts constantly generate new cells that migrate towards the central canal. In doing this they obtain different tasks, and at the same time maintain and renew the barrier and layer of cells within just a few days under healthy conditions.
This regenerative capacity is very useful when the barrier gets minor damages that can then quickly be repaired. Together with the immune system and the gut microbiome a harmonious balance of gut health is generated. A balanced and fiber-rich diet (remember the apple!) keeps the bacteria happy, so that they produce molecules that our body needs.
While the molecular details are still unclear in many cases, we know that the right microbiome composition is needed for a healthy physiology, not only in the intestine but amazingly enough also in distant organs like the brain and lungs.
Read also the part 2 here: https://blogit.utu.fi/inflames/en/2023/01/25/gut-feeling-part-2-butterflies-in-the-stomach-or-something-serious/

Diana Toivola, Associate professor at Åbo Akademi University
Faculty of Science and Engineering, Biosciences, Cell Biology

